Rubella Symptoms, Prevention, Causes And Treatment
621
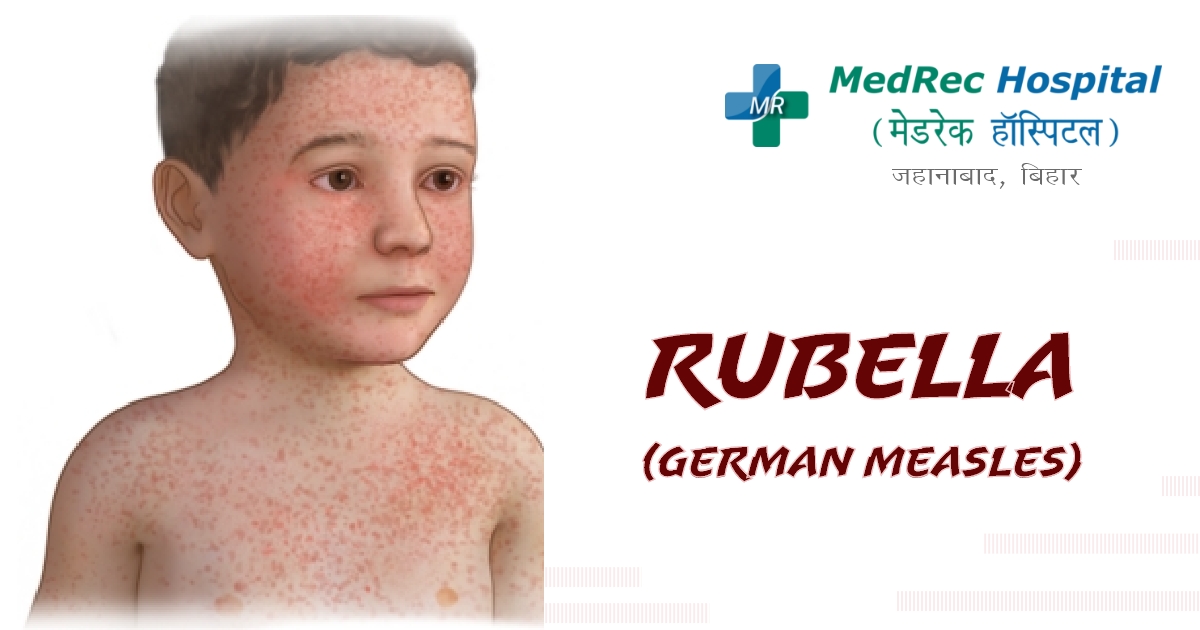
The red rash that characterizes rubella, a common viral illness, is its most distinguishing feature. Other names for it include German measles and three-day measles. Most people may only have minor symptoms from this virus. But, if a mother has the infection while she is pregnant, it can seriously harm the unborn child.
Although rubella and measles are different diseases, they do have certain similarities in their signs and symptoms, such as the red rash. Rubella is not as contagious or harmful as measles and is brought on by a separate virus.
The measles, mumps, and rubella (MMR) vaccination prevents rubella safely and effectively. Immunization offers lifetime immunity against rubella.
In many nations, cases of a rubella infection are few or nonexistent. The virus still exists, though, since not everyone uses the vaccination. creates severe issues for children whose moms contract the infection while pregnant.
Causes
A virus that spreads from person to person is the cause of rubella. When an infected individual coughs or sneezes, it can spread. Direct contact with contaminated nasal and throat mucus is another way it can spread. Moreover, it can travel through the bloodstream from pregnant mothers to their unborn offspring.
A person who has been exposed to the rubella virus is contagious for about a week before the rash appears and for another week after the rash has disappeared. An infected person might spread the illness before realising they are sick.
Due to widespread childhood vaccination programmes against the virus, rubella is uncommon in many nations. In several regions of the world, the virus is still present. Particularly if you are expecting, this is important to think about before travelling overseas.
After contracting the illness, you are often immune for life.
How to check if you have Rubella?
If you suspect that you or your child may have been exposed to rubella or if you detect any symptoms or indications that might indicate rubella, get in touch with your doctor right away.
Check your immunization history to confirm that you have had the MMR vaccine if you are thinking about becoming pregnant. If you have rubella while pregnant, especially in the first trimester, the virus may kill the fetus or result in severe birth abnormalities. Congenital deafness is most frequently caused by rubella during pregnancy. The best time to obtain rubella protection is during pregnancy.
You will probably go through a standard examination to check your immunity to rubella if you are pregnant. But, if you have never had the vaccination and believe you may have been exposed to rubella, call your doctor immediately.
Symptoms
Rubella symptoms and indicators can sometimes be overlooked, especially in young children. After being exposed to the virus, signs and symptoms often start to show two to three weeks later. These include:
- Moderate fever of 102 F (38.9 C) or below
- Headache
- Runny or stuffed nose
- Red, itching eyes
- Big, sore lymph nodes behind the ears, at the back of the neck, and the base of the skull
- A little, pink rash that starts on the face, moves fast to the trunk, then the arms and legs, and eventually vanishes in the same manner.
Prevention
The MMR vaccination, which protects against measles, mumps, and rubella, is typically administered. This immunisation may contain both the MMRV vaccine and the varicella (chickenpox) vaccine. Doctors recommend that children take the MMR vaccine twice, first between the ages of 4 and 6 years and again between the ages of 12 and 15 months, prior to entering school.
The MMR vaccination provides lifelong immunity against rubella and prevents it.
Infants born to moms who have received the vaccination or who are already immune are often protected from rubella for 6 to 8 months after delivery. The rubella vaccination can be administered as early as 6 months of age if a child needs protection from the disease before the age of 12, such as for specific international travel.
Combining recommended immunisations, such as the MMR vaccine, can minimize delays in measles, mumps, and rubella protection while requiring fewer injections. The combined vaccination is equally secure and efficient as the vaccines are administered separately.
There is no evidence linking the MMR vaccination to autism. Concerns regarding a potential connection between the MMR vaccination and autism have been widely expressed. There is no scientifically established connection between the MMR vaccination and autism.
Several groups point out that autism is frequently discovered in toddlers between the ages of 18 and 30 months, or about the time when children receive their first dose of the MMR vaccination. Yet, this time coincidence should not be interpreted as a cause-and-effect link.
You do not need a vaccination if you:
- Received two doses of the MMR vaccination after turning 12 months old.
- Do blood tests to verify your immunity to rubella, mumps, and measles.
- Born before 1957. Individuals who were born before 1957 are likely immune since they were exposed to measles, mumps, and rubella as children. The MMR vaccine is advised, nonetheless, in the absence of a blood test that demonstrates immunity.
- If you have not had two doses of the MMR vaccination by the age of 12 months or a vaccine, get one.
- A blood test to confirm your immunity to rubella, mumps, and measles.
The vaccination is not advised for:
- Women who are pregnant or who want to get pregnant within the next four weeks
- Individuals who have experienced a potentially fatal allergic response to gelatin, the antibiotic neomycin, or an earlier dosage of the MMR vaccination
- Talk to your doctor before having the MMR vaccination if you have cancer, a blood issue, another illness, or you use medicine that weakens your immune system.
The majority of people do not have any adverse reactions to the vaccine.
Some adverse effects may develop for some people two weeks after immunisation, although they typically happen less frequently after the second injection. They may consist of:
- Sore arm at the injection place
- Fever
- Mild irritation or redness at the injection site
- Particularly in teenagers and adult women who had not previously developed immunity to rubella, temporary joint discomfort or stiffness
- Glands in the cheeks or neck swelling
- Seizures brought on by a fever
- Rash all over the body
- Severe allergic response
Following a diagnosis
If you have rubella, you can help keep your friends, family, and coworkers safe by informing them of your diagnosis. Inform the school or nursery if your child has the rubella virus.
Treatments
Therapy cannot shorten the course of the rubella infection, and since symptoms are commonly mild, usually no treatment is required. During the contagious time, however, medical professionals often advise seclusion from others, particularly pregnant women. As soon as rubella is detected and for at least seven days after the rash goes away, isolate yourself from other people.
Depending on the severity of the infant's issues, support for a child with congenital rubella syndrome varies.Early treatment from a specialised team might be beneficial for children with many challenges.
Complications of Rubella
Rubella is a minor infection. Rubella can cause arthritis in the fingers, wrists, and knees in certain women, which typically lasts for approximately a month. In rare situations, rubella might result in an ear infection or brain inflammation.
But, if you have rubella while pregnant, it might have a serious and occasionally deadly impact on your unborn child. Congenital rubella syndrome affects up to 90% of children born to moms who contracted rubella during the first 12 weeks of pregnancy. This syndrome may result in one or more issues, such as:
- Delays in Growth
- Cataracts
- Deafness
- Heart development issues (congenital heart defects)
- Issues with the growth of other organs
- Issues with learning and mental development
- The first trimester is the most perilous time for the foetus, although exposure later in pregnancy is still harmful.
For further information please access the following resources:
Emergency : +91 89686 77907
Front Desk : +91 98018 79584
Page last reviewed: Jul 12, 2023
Next review due: Jul 12, 2025







.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)